Introduction
Hypertension is a worldwide public health problem.1It is becoming a global epidemic in all age groups, and both the rural and urban settings.2Globally, more than one billion adults are hypertensive and this is predicted to increase to 1.56 billion by 2025.3Existing evidence shows a global prevalence of 22%, with a considerable variation from country to country.4In Sub–Saharan Africa, it has been estimated that the prevalence is highest with about 46% of adults aged 25 years and older being hypertensive.5In Ethiopia, its prevalence ranges from 15.6% to 28.3%.6–10
Uncontrolled hypertension leads to severe cardiovascular diseases, renal failure, and mortality.11High blood pressure is associated with at least 7.6 million deaths per year worldwide (13.5% of all deaths), making it the leading risk factor for cardiovascular diseases.12Recent data in Ethiopia also showed that hypertensive stroke is the leading cause of death in the country.13
Previously, hypertension was said to be a disease of the rich. However, as a result of the epidemiologic transition, the disease burden shifts from richer and better-educated segments of society to the poorer and less educated ones.14Advanced age; male gender; behavioral factors such as high salt intake, obesity, harmful alcohol consumption, and tobacco use; and work–related factors such as stress and sedentary behavior have been implicated in the etiology of hypertension.15–17Moreover, an unhealthy diet due to nutritional transition and adoption of westernized dietary habits such as greater consumption of processed foods which are high in salt, fats, and sugars are contributing factors.15In Ethiopia, higher salt consumption has been recognized as the main risk factor for hypertension. A study in the capital city of the country reported an estimated mean salt intake of 8.3 gram/day, which is higher than the World Health Organization recommendations of 5 gram/day.
Hypertension is both preventable and manageable diseases.17Hypertension self-management skills, including blood pressure self-monitoring, lifestyle changes, adherence to medications, and shared medical decision-making represent a cornerstone of recommended care for hypertension and have been associated with significant improvements in hypertension control among treated patients.18A well-controlled blood pressure is an important indicator of effective health care delivery and self-management skills.1Patient experience with the quality of health care is associated with patient safety and clinical effectiveness for a wide range of disease areas.19Better patient experience with the quality of health care is associated with better adherence to prevention and treatment recommendations, and better clinical outcomes.19,20
The increasing prevalence of non-communicable diseases coupled with a high burden of communicable, nutrition, maternal, and childhood diseases challenge the existing health system.5This challenge is prominent in the Sub-Saharan context where the health system is inadequately prepared to control and manage chronic conditions, including hypertension.21Managing a rising demand for this challenge is difficult both for physicians and policymakers across health systems in the region. Often, patients with hypertension in this region lack access to optimal health service and eventually face a looming crisis due to poorly controlled hypertension.13
Evidence shows, for effective management and control of hypertension, the patient should have enhanced self-management skills and get adequate support from care providers and the health system at large.22However, the self-management behaviors, including blood pressure self-monitoring, lifestyle changes, adherence to medications, and shared medical decision-making with care providers is inadequate.10Further, hypertensive patients may possess an inaccurate or incomplete understanding of hypertension, the process and goals of hypertension care, and their role in managing hypertension.23Moreover, patients may lack the required support from health care providers while practicing hypertension self-management,24which in part may be attributed to prescribers’ behavior, competencies and large patient-prescriber ratio.23
Although health care quality is critical to enhance the self-management behaviors and improve clinical outcomes for the growing number of hypertensive patients, the issue has not been fully elucidated in the Ethiopian context. Managing a rising demand for the challenge faced both by physicians and patients across the health system needs evidence like this. Therefore, this study intended to explore the experience of hypertensive patients in self-management practice and the quality of health care in a public hospital located North-west of Ethiopia.
Patients and Methods
This study was conducted in Felege Hiwot Comprehensive Specialized Hospital which is located in Bahir Dar City, north-west Ethiopia. It is a public hospital which was officially commenced its function in 1963 as a district hospital and then upgraded to a referral hospital in 1994. The hospital is staffed with 600 health workers and equipped with around 400 beds and 9 operating tables serving over seven million people. It provides obstetrics, pediatrics, general surgery, internal medicine, ophthalmology, gynecology, intensive care units, and orthopedic surgery services. In the hospital, there are 672 patients on hypertension follow as at the time of the study. Hypertension is the leading cause of morbidity among the chronic diseases and the second among the ten top diseases in the hospital according to the 2018 report of the hospital.
A qualitative study with a phenomenological approach was employed. Phenomenological research design enables researchers to describe the lived experiences of individuals about a phenomenon. This approach focuses on describing what participants have in common as they experience a phenomenon.25
The participants of this study were both men and women hypertensive patients on treatment follow-up at the hypertension clinic of a public referral hospital. Participants were selected purposively using the maximum variation technique to gain insight from a wide range of perspectives and to document important shared experiences that cut across the different characteristics. Patients were selected by considering their difference in educational status, residence, gender, and blood pressure control status (either controlled or uncontrolled high blood pressure). Maximum Variation Sampling involves the selection of a wide range of cases to document the diversity and identifying important common patterns that are common across the diversity of dimensions of interest.26Nurses working in the clinic were involved in the process of selecting the hypertensive patients who can provide a rich pool of information.27The inclusion criteria for patient participants were, being on antihypertensive therapy follow–up for the past six months prior to the study; aged 18 – 65 years, and able to speak the local language.
Eleven patients were recruited for the in-depth interviews by considering the above variations. Table 1 shows the characteristics of the 11 participants involved in this study.
Table 1 Sociodemographic Characteristics of the Study Participants |
Two key informant interviews were also conducted. Even though we approached both nurses and doctors to participate in the interview, only nurses were voluntary to participate as key informants in this study. The final sample size for the in-depth interview was determined based on the notion of saturation with no new issues or ideas emerging from the participants.28
An in-depth interview was conducted from May 6 to 17, 2019 by the researchers using a semi-structured interview guide that is designed to elicit participants’ perspectives via open-ended questions that probe to trigger more exploration. In-depth-interview is a commonly used method to describe the experiences of individuals about a phenomenon.27To triangulate the data obtained through the in-depth interview, key informant interviews were conducted with two nurses working in the hypertension care clinic.
Patients were approached while they waited for their appointment, and were questioned briefly by nurses to determine whether they fitted the selection criteria and the required patient characteristics. Participants were interviewed by the investigators within the hospital premises after completing their appointment checkups. Interviews were conducted in the local language. The questions were developed by the researchers after reviewing previous studies conducted on related topics. The interview guide was refined further as we continued conducting the interviews. It mainly focuses on patients’ understanding of hypertension and the self-management practices, their experiences with antihypertensive medication adherence, physical activity, diet adjustments, blood pressure monitors, and the reasons for not following the hypertensive care recommendations. It was also designed in a way to explore the experience of hypertensive patients with the quality of health care they receive in the hospital. Interview guide is attached asSupporting Information (S1andS2). At the time of the interview, all the conversations were audio recorded using a smartphone with the permission of the participants. While one of the investigators conduct the interview, another investigator takes field notes during the interviews to capture nonverbal information that cannot be captured by the audio records.29The duration of the interviews last between 30 to 60 minutes.
The data from the interviews were transcribed verbatim into Amharic by the investigators together. Transcripts were verified by the researchers for their accuracy by listening to the audio records and field notes were checked in the transcription process. The finalized transcripts were translated into English. The data were analyzed by the investigators using thematic analysis. The open code software was used for the analysis to assist and to facilitate the coding processes, and further categorization was made to make sense of the essential meanings of the phenomenon and to allow the emergence of the common themes.
We employed an inductive approach for analyzing the data with no predefined framework. The actual data itself was used to derive the structure of the analysis. The primary investigators generated initial coding schemes independently, and differences were resolved through discussion. Once agreed on the coding schemes, the investigators categorized codes into sub-themes and themes independently again. The lists of categories by the investigators were then compared with an on-going dialogue, and adjustments were made accordingly.
We used different data sources to triangulate. Having the data analyzed by two or more persons independently and comparing their findings would increase the credibility of our findings.29To ensure credibility, we had prolonged engagements in reading and analyzing the transcribed data. The study was conducted under the supervision and with the continuous guidance of an experienced qualitative researcher that insured the dependability of the study. In qualitative research, dependability often refers to the stability of responses to multiple coders of data sets (intercoder agreement).27We assessed the consistency of the emerging codes among coders. We have a detailed description of the research process to enhance its understanding by the readers. We have a rich, thick description of the participants of the study, as well as a detailed description of the findings with adequate evidence presented in the form of quotes from participant interviews, and field notes.28The research team met regularly for reflexive discussions which helped us to be aware of our thoughts and assumptions and minimize the potential effect of these on the process and findings of the study. The researchers have previous work experiences in public health facilities, hence were not challenged in conceptualizing the research question that is relevant to participants’ experience. However, none of them have been working in the study hospital.
This study was approved by the Ethical Review Committee of the school of public health, college of medicine, and health science in Bahir Dar university. Further permission to conduct the research was obtained from the authorities in the study setting. All study participants were informed about the objective and nature of the research prior to the data collection. Verbal informed consent was secured from each of the study participants. Verbal informed consent was approved by the ethics committee, and the participant consent included publication of anonymized responses. Convenient spaces were arranged within the hospital compound for the interviews to protect the privacy of participants. To compensate for the opportunity cost of time spent on the in-depth interview, pocket money of 58.00 Ethiopian Birr (equivalent to exchange rate of US$ 2 at the time of the study) was provided to each participant.
Results
The participants of the study included 11 patients attending the hypertension care follow up and two nurses working in the chronic care unit. Four male and seven female hypertensive patients with age ranging from 35 to 65 years participated in the study. Only seven of them had a well-controlled blood pressure of below 140/90 mmHg at the time of the interview. Other characteristics of the participants are shown in Table 1.
During the analysis of the interviews, two main themes and seven sub-themes were identified. The first theme “experience in self-management practice” describes medication adherence, lifestyle modification, and self-monitoring of blood pressure. The second theme “experience in the quality of health care” discusses access to health services, patient-centered care, the behavior of health care providers, and time and patient flow management.
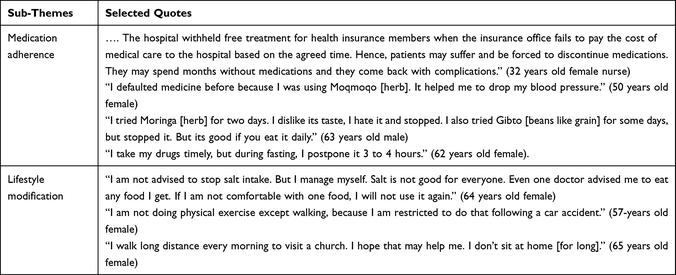
This theme describes the level of patients’ adherence to prescribed medications, lifestyle modification, and self-monitoring practice of their blood pressure. Additional patient experience quotes related to self-management practice are described under Table 2.
Table 2 Patient Experience Quotes Related to Self-Management Practice |
Some participants found taking medicine is always burdensome. Some of them also had limited knowledge about the treatment and are doubtful about the effectiveness of the antihypertensive medications. They take them because they are told not to stop by the health care providers. About one-third of them had stopped the medication because they thought that traditional medicine could cure the condition and they tried different herbal or religious alternatives. Missing doses and delay in taking the medicines are also common. The use of alternative traditional treatments and being desperate about the usefulness of medicines in treating their disease condition were the most common reasons for defaulting and poor compliance. One of the participants missed doses of medicines when she was unable to get breakfast before taking the medicines. She believes that taking the medication before a meal could harm her health.
“I went to Lalibela [a holy place] and stayed for almost a year. During that time, I did not take the medicines. It is unusual to take medicine when you are in holy places, but there is no restriction. I came today after I have been living without medicines for the last one year.” (65 years old female)
“One person told me that Grawa [herb] is good [for treating hypertension]. I drunk it and I feel when it drops my blood pressure. It [the herb] reduces blood pressure.” (64 years old female)
“ …. The drugs are useless; they cannot cure you. But I will take it because I have to live longer for my daughter.” (50 years old female)
“I have many diseases, I have diabetes, blood clotting, gastritis, asthma, and hypertension. I am taking medicines for all of these diseases. Sometimes, I could not take medicines according to the order of physicians because things are not always good at home. You may need to have breakfast before taking medicines, but you may not get it on time. When it is available, it may not be salt-free. It is difficult.” (50 years old female)
One patient had defaulted the medicines because she was free of the symptoms and feeling healthy. She stated that she has no idea about the importance of the medicines and how to comply with them. She could not get ongoing counseling from the health care providers during her follow up visit.
“When I feel I am okay, I stop the medicines. Initially, I wasn’t told about the importance of taking medicines always. The doctors measure and write to me only the prescription, I don’t have any idea about how to take or comply with medicines.” (60 years old female)
Financial difficulty was also a reason for some of the participants to stop medication intake. This reflection was also corroborated by one of the nurses interviewed. A participant revealed that at one time she had stopped the medication because of financial difficulty to cover the cost of medicines. Initially, the cost of her treatment was covered by a fee waiver. When she was excluded as a fee waiver beneficiary, she could not afford the cost of her treatment.
“I was taking drugs for free. However, the Kebele [local public leaders] excluded me from the fee waiver membership for the reason I didn’t know. At that time, I had no idea about how to get money for the drugs and I was forced to stop taking the treatment for a reasonable period.” (62 years old female)
“Sometimes, although patients may have insurance coverage, medicines may not be available in the hospital. In this case, patients would be given prescriptions to buy drugs from private pharmacies. However, they may not afford to buy drugs outside and leave without having it [medicine]. That is also another reason for defaulting.” (32 years old female nurse)
One participant regretted for taking the antihypertension medication because other patients whom he knows are living well without the medication only by lifestyle adjustments. Moreover, when he consulted the health care providers about the possibility of stopping the medicines, he was “misinformed.”
“There are some problems with doctors. They simply give you the medicines without looking into other alternatives. Some people threw their medicines away and are living well just by minimizing salt intake. I wish I could do the same. But, when I asked the doctors the possibility of stopping the medicines and manage it by minimizing salt intake, they said ‘it was possible before, but once you started the medicine, there is no option to stop it’. Had they told me that it is possible to live without the medication, I would not have started the medication.” (63 years old male)
One of the participants had difficulty in differentiating the antihypertensive medications from medicines prescribed for other comorbid conditions.
“I am taking many drugs for a heart problem, diabetes, hypertension, anticlotting, and hemorrhoid. I had taken the wrong drug assuming it is the antihypertensive drug and collapsed. I have many drugs in my home, I forget things, including dosages and types of drugs. If I see the drugs together, I couldn’t differentiate and may take them wrongly.” (65 years old female)
Some participants revealed that they are taking their medications without interruption with a slight deviation of the right time. One patient indicated that she delays the timing of taking the medicines because of fasting, while another one does the same thing because of fear of drug-drug interaction. For a few of the participants, taking medications regularly is not a challenge.
“I take my drugs regularly; I never had defaulted them.” (57 years old male)
Eleven of the participants were aware of the importance of salt restriction or reduction in managing their blood pressure. However, one of these still did not reduce salt consumption although he knows it as a risk factor for hypertension. This patient believes that his health condition is improved after starting medication hence continue to consume salt. Two participants claimed that they are not consistent in using salt-free foods especially when they are invited to social events. Two participants revealed that they were not advised by the health care providers to restrict or reduce salt intake, but they manage it based on the information they get from other sources. Even though she has limited salt consumption at the time of the interview, one participant found it difficult to adapt to a salt-free diet initially after being diagnosed with hypertension.
“When I go to attend social events, it is hard for me to get a salt-free diet. Salt is not good for everyone.” (60 years old female)
“ …. it is difficult to eat foods without salt. I lose resistance when I was eating foods without salt for two months. I suffered a lot. Then I decided to add a small amount of salt to the food.” (35 years old female)
Drinking alcohol is not the concern of most participants. Two of them did drink alcohol even before they were diagnosed with hypertension, while others either stopped or limited the use of alcohol. Only two patients disclose that they are using alcohol [Tella - local alcohol drinks].
“I take drinks except for Araki. I drink Tella, the one which stayed for a longer time. If it lasts more than 2 weeks, no problem. The problem is with the fresh one.” (51 years old male)
Concerning weight control, only three participants are aware of the benefit of limiting fatty meat and reduced it in their diet. Whereas two of them stated that they have limited use of sugar and sweaty foods. The benefit of regular exercise is known by most of the participants. However, about half of them are not doing it for different reasons. Only two participants said that they exercised regularly and according to the recommendation. One participant was aware of the benefit of physical activities for his hypertension management, but he claimed that he was too busy with his work and daily life commitments. He said it is not convenient to do regular exercise. Three participants felt that it was unsafe for them to exercise or to walk outside their houses. Two of them are due to mobility difficulty as a result of the disease complication while the other one is due to injury on her back after a car accident and she is not walking regularly as the time she enters to and leaves from the workplace is not convenient. Although she recognized the importance of physical exercise, she was scared of further injury or recurrence of her back. However, she stated that she tries to walk outside her home in other opportunities like when invited to social gatherings.
“I used to do physical exercise like jumping and others before I faced the car accident. But after the accident, I could not jump because my back was injured. I don’t want to try it. But as much as possible I travel on foot particularly when I go to church, social gatherings, and hospital. I use vehicles to go to a workplace because the time is not convenient to walk on foot.” (57 years old female)
“I do regular exercise for one hour every morning. (57 years old male)
None of the participants use home monitors to check their blood pressure. The frequency of monitoring is based on perceived need (when they see symptoms). Most patients reported having their blood pressure measured opportunistically when visiting their health care providers, approximately every four months.
“Sometimes the symptoms disappear and sometimes they reappear. When I see the symptoms, I go to private clinics to measure my blood pressure.” (64 years old female)
“I check my blood pressure in students’ clinic. I used to check every week, then every two weeks, until it was controlled.” (35 years old female)
The participants raised concerns regarding the health care system most of which are barriers to the self-management of hypertension. This theme includes four subthemes: access to health services, patient-centeredness, health care providers’ conduct, and time and patient flow management. Additional patient experience quotes related to the quality of health care are described under Table 3.
Table 3 Patient Experience Quotes Related to the Quality of Health Care |
This sub-theme includes the availability and cost of medicines, affordability of the cost of medicines, and availability of the required manpower. Availability and cost of antihypertensive medicines within and outside the hospital environment appeared to be a deterrent condition for the clients’ adherence to medication protocols. Availability of medicines within the hospital depends on the type of medicine. Some patients might get all the prescribed medicines while others could get partially or not at all. The cost of medicines is increasing from time to time, and the problem is more critical in private pharmacies. With this condition, most patients could not afford the cost of medicines and are often tempted to stop their treatment.
“The cost of medicines is increasing. The price is now doubled compared with the one when I started the medication. Especially, when medicines are not available in this hospital, we opted to go to private pharmacies, it is very, very high there. When medicines are prescribed for three or four months, the cost could be as high as 4000 to 5000 Birr (US$139.6–174.5). Since I have a monthly salary, I afford the cost; I buy the medicine without any problem. For many patients, it is difficult to afford the cost. They may stop the medication.” (57 years old female)
“It [the cost of medicines] is difficult. I bought each pill for 7.80 Birr. I never get it from this hospital, I always buy it from private pharmacies. Ok I may afford it, but what about others, they will die! The cost is high.” (60 years old male)
Fee waived patients and those having community health insurance coverage, do not have a financial hardship to cover the cost of medicines. However, if medicines are not available in public hospitals, then they will face a high cost of drugs to procure from private pharmacies.
“Insured patients come here with the anticipation that all of the drugs they may need are available in the hospital. But that is always not the case. Often, particularly on current dates, patients are having difficulty in getting some or most of the prescribed drugs in the hospital. In this case, they will be given prescriptions to buy on their own. Because they don’t bring money, they will return home without medication. Either they return with money to buy prescribed drugs outside or disappear from follow up.” (28 years old female nurse)
Participants are not convenient with the type of health care providers working in the chronic care clinic. One participant stated that they could not able to get the consultation of senior physicians while another emphasized that only internship students are providing care without the direct supervision of experienced physicians.
“I am not happy. We need senior doctors to treat us. We are not getting opportunities to talk to senior physicians, we simply get a refill.” (57 years old male)
This subtheme includes issues like patient counseling, listening to the concern of patients, the caring and compassionate attitude of health care providers, and information exchange between health care providers and the patients. Regarding patients’ views on the health care providers’ attitude, the majority of the patients stated that they are not satisfied with the way health care providers deal with them. They indicated that they could not get ongoing counseling from the health care providers during their follow-up visit. They also expressed that they received incomplete and/or no information from the health care providers regarding hypertension and its treatment.
“The doctors measure [my blood pressure] and write me only the prescription …. Initially, I wasn’t told the importance of taking the medicines regularly.” (60 years old female)
“There is no counseling. Truly what we have learned in school is not practiced here. We can advise many things like food …. Counseling is more helpful for the patient than medicine, I mean psychological support. But there is no counseling here. I told you, he prescribed the medicine for four months, then I go, that is it.” (35 years old female)
Consistent with this idea, the two nurses working in the chronic care clinic indicate that they could not provide ongoing counseling for their clients because of a high patient-provider ratio. However, one of the participants recommended that nurses should use the opportunity to provide health education in the morning while patients are waiting for the service.
“Patients are right, we do not have time to teach and advise them, the patient – care provider ratio is very high. We are busy. That is why we do not teach them one by one.” (32 years old female)
“We are not getting health education; we spend more than two hours waiting for the physicians to come. Nurses could teach us in the meantime, but they never do that.” (57 years old male)
Participants indicate that health care providers are not willing to address their needs and listen to their concerns. They emphasized that physicians are not listening to them. Patient complaints unrelated to hypertension could not get the attention of health care providers.
“We need the doctors to listen to us. But while you are talking to them you often see their attention is away from you or they may be talking to other patients. I get angry about this situation. The treatment isn’t complete, without your concern being listened to. When I talk to you, I get relief.” (65 years old female)
“ …. when I ask them [the doctors] to order me laboratory tests, they say they don’t do that here and told me to go to private clinics. Today I have throat pain and difficulty in swallowing, but the doctor only pretends to have checked it and ignore it. He should have referred me to the senior.” (65 years old female)
It was understood that the patients expected more questions from the physicians about their health status, medicine adherence, the side effects of the medicines, and other relevant issues. They wanted to express their concerns to the physicians. However, they could not freely discuss their health status and the physicians do not ask either. They stated that the physicians prescribe medicines only based on blood pressure level without seeking further information from the patients. Patients are not also informed about their checkup results. The participants highlighted that they have little consultation time, a key problem faced during their visits to the health care providers.
“I come every four months. No one asks you about how you spent the four months, we simply get a refill. They [the Doctors) come very late and when they get started the service, they do not give proper management, they rush.” (57 years old male)
“I never get health education; no one asks or listens to you. They [the Doctors] simply see your chart, flipping the pages like a judge and write something.” (65 years old female)
Participants raise a concern about the safety and caring attitude of the health care providers. Two participants stated that medical error is a common problem within the hospital and one of them has experienced this problem– she was given the wrong medication two times. For this, health care providers are not trusted by their clients.
“They [doctors] don’t take care of you. I was diagnosed suddenly. I was referred to this hospital with a blood pressure of 170/112 mmHg. It was too high and needs emergency management. But the first doctor gave me only HCT. I was doubtful and went to another doctor. When he examined me, it was indeed high and I was admitted to take Hydralazine IV. I was saved because I am a health professional. Imagine what a layperson will do in such circumstances. (35 years old female)
“I was given the wrong medication two times while I was admitted to this hospital. One of the health care providers gave me the wrong medicine. Then I was changed, I was burnt, I threw my closes, I became mad. Then the doctors gather ….” (64 years old female)
“The doctors working in the emergency department have a very serious problem. They could give you a wrong injection, you know, I have seen a woman died because of this error, “oh my God! No matter how it helps or kills you, they will give you an injection, I don’t trust them.” (50 years old female)
The participants also believe that doctors are not empathetic and compassionate. They are not willing to understand the feelings and problems of their clients. Patients could not get reassurance from the physicians in case of a severe disease condition.
“ …. If we don’t come on the appointment date, it is difficult to get the service. We cannot get our medical records without the willingness of the doctor. First, we should tell the reason why we miss the appointment date to the doctor and get his willingness to receive the service. It is a long process. There are convincing reasons to miss the appointment date, like lack of transport, funeral events, and others, but they don’t understand you.” (57 years old female)
“I was admitted to emergency ward failing to control my urine, half-paralyzed and I heard the doctor saying ‘she will not survive but, let us try’ thanks to the Lord, I am still alive. I did not think that I would survive.” (50 years old female)
The behavior of health care providers becomes another deterrent to the patients’ self-management practice. Patients emphasized the rude and non-friendly behavior and attitude of health care workers as one of the key barriers of self-management practices. Patients received ill-treatment, embarrassed, insulted, and intimidated by health care workers.
“People working in the card room and laboratory unit do insult me, they embarrass me; and warn me to get out of the area. There are many problems in the laboratory unit [angry and emotional], they are rude [with load voice]. They insult me “dirty woman.” (50 years old female)
“ …. Even the gatekeepers are difficult people in their own, they intimidate and embarrass you, they push you.” (65 years old female)
The health care providers are not polite during a patient consultation. They become emotional when patients are not following their recommendations. They are using harsh words rather than trying to identify the reason why patients are not adhering to their treatment and other recommendations as stated by one of the participants.
“I came today after I have been living without medicines for the last year [in Holy water]. When I inform the doctor, he said, ‘why you came? You better stay there and die alone’. I had no answer, and remain quiet. … it was better not to come back; I was healthy there [in the Holy water].” (65 years old female)
Participants are also concerned about the unequal treatment of patients within the hospital. They stated that providers especially people working in the medical registration unit are disrespectful of laypeople. They discriminate against people because they are farmers or are not well dressed.
“Medical record unit staffs are disrespectful of patients. Especially they don’t treat patients equally. They discriminate against patients who are farmers. They discriminate against people because they are not well dressed. Every patient should be treated equally. Patients should be respected because they are human beings ….” (35 years old female)
Patients are discouraged by the long waiting time during their follow up. They wait endlessly until they get the service in different units of the hospital including the chronic care follow-up clinic, pharmacy, and cashers. As outlined by the participants this problem is because of either the doctors are coming late or they leave the clinic early. The shortage of manpower and poor management of the patient flow also aggravates this problem.
“I came early in the morning, but I get the service now at 11.00 am. The doctor enters at 9.00 am. I think he may be working in a private hospital. The hospital is almost forgotten. Even I am better but inpatients are in difficult conditions. If you see them, you will cry, no one sees them.” (62 years old female)
“You cannot get the service timely even if you come early. They may be overloaded. But they don’t consider the order of patient arrival. The one who comes first may be served at the end and the one who comes late may be served first.” (35 years old female)
Discussion
This study explored patients’ experiences of self-management practice of hypertension in a public hospital in North-west Ethiopia. Another objective of the study was to explore the role of health care quality in facilitating the effectiveness of the self-management practice of hypertensive patients. Pill burden remains challenging for some of the patients. Apart from facing a heavy burden by taking many drugs at a time, some of the patients have difficulty in identifying and differentiating medications. Hence, they tend to take drugs wrongly and experienced severe symptoms such as fainting, confusion, and altered daily functioning.30As reported by a previous study, patients were unable to recognize which was the antihypertensive agent when more than one type of medicine is prescribed for comorbid conditions.31
This study showed that most patients have either missed doses or stopped taking the medicines at one time in their experience with the disease. The factors that influence the patients’ adherence towards their medication were explored. Reliance on traditional medicine, beliefs that the medicines could not be taken by an empty stomach, being free of the symptoms, financial difficulty to cover the cost of medicines are some of the main causes of medication non-adherence or to stop taking the medications. Patients postpone the time of medication because of fasting. As reported by other studies, religious beliefs had a strong impact on the patient’s adherence to medicines.32,33In Malaysia, the majority of patients stated that diseases can be cured with amulets, sacred water, and religious treatments.32Economic problems,34,35and a lack of symptoms or diagnoses of “normal” blood pressure36were also reported as reasons for decisions on medication use.
Some patients considered hypertension as an uncontrollable condition and stated that it is useless to use medicines as there is no cure and it always becomes worse with time.32This feeling of despair is also explored in our study. Literature also shows other reasons for lack of adherence to medication, including experience of medication side-effects, and fear of side-effects,34,36life responsibilities and lack of family cooperation;35and treatment durations, inconvenient dosing, and beliefs that medications are addictive and cause impotence.34The findings of the current study generally indicated that the patients’ lack of ongoing education and counseling is the main root cause of poor medication adherence.
Dietary management was also a challenge for most of the patients. Some had a lack of family and social supports in understanding their problem and in preparing a salt-free diet. Attending social events is difficult as food preparation does not account for their condition. A similar finding was reported in Malaysia were complying with low salt and low-fat diet was difficult due to the lack of family and peer support.37The challenge of adapting a salt-free diet was also reported by another study.38
In the current study, participants reported that the health care system is creating barriers to make the appropriate decision and employ effective self-management practices. A lack of access to medicines in hospital stocks and the lack of money to cover the cost of medicines is reported as a barrier for hypertension medication adherence. They are facing a high cost of medicines in the private pharmacies because of the scarcity in the public hospital. As explored by similar studies, patients reported that they were struggling to pay for the cost of hypertension medications.33,39Another study identified that sometimes the medicines are not in stock in the hospital, ultimately ended up buying them from a private pharmacy which proves costlier to them. The problem seemed especially critical when medicines are expensive.40
Good provider-patient relationship is reported to be important for people to return for clinic visits and engage in self-management practices. Participants who were adherent described their physicians as honest, caring, listening, or a friend.34However, in our study, almost all participants described that care providers do not listen and respect them. Patients felt that their concerns are not heard and perhaps ignored. Patients specifically wanted health care providers to spend more time explaining their condition, to provide practical guidance on self-management, and to listen to their concerns. However, participants were concerned about the health care providers’ lack of interest to elicit information from patients, addressing the full range of patient needs, and listening to them. They could not receive adequate information; counseling or education on self-management practice from their health care providers. The lack of this necessary knowledge puts them at a significant disadvantage for managing their condition. Participants reported several misunderstandings due to not receiving the required information. These included the patients’ doubts on the effectiveness of medicines, as well as beliefs on alternative traditional medicine to control hypertension.
The providers’ failure to establish a sense of relatedness with their patients including not having the time to ask, listen, or to counsel the patients on self–management is also reported by other studies. Insufficient information and understanding is a major barrier to medication adherence.32Patients were not encouraged to express any response or opinion.41The doctor’s consultation time with them was too short even after hours of waiting in the queue.32,34,40–42The lack of time for patient-physician consultations seems due to the heavy workload, and this is supported by other similar studies.31,40Some participants accepted the lack of information from the physician as normal because they understood the doctor’s heavy workload.31Those who received limited information from the health care providers reported that the information provided seemed to focus only on blood pressure readings, without further explanation on how this is connected to their medicines or other management.31
Participants also believe that physicians have not a caring, empathetic, and compassionate attitude towards them. Two patients shared their experience of medical error while they were admitted to the hospital. They were not receiving polite words when they fail to adhere to their treatment or other recommendations. For this, health care providers are not trusted by some of the patients. A similar finding was reported by Murphy et al in South Africa, where patients felt that they are not understood, cared for, and valued by their health care providers. Distrust of health care providers by some care recipients was also evident because of the absence of behaviors perceived as communicating, caring, and partnering.41
Participants of our study pointed out the rude and non-friendly behavior and attitude of health care workers. They believe that they are not treated like humans, they are embarrassed, insulted, and intimidated by health care workers. This concept is reported by other studies as one important barrier for self-management of hypertension.32,41Patients described how the negative attitudes of health care providers inhibited their ability to be open with and trusting of them. Patients complained about nurses, in particular, being impatient, abrupt, and disrespectful.41
Limitation of the Study
This qualitative study is the first of its kind in exploring the self-management practice of patients with hypertension and health care system barriers to self-management practices in Ethiopia. We tried to enroll diversified patients in terms of age, disease control status, educational status, and gender. However, the study was confined to a single public hospital. Recruiting patients from other public or private hospitals might have given a different perspective. Moreover, organizing a focus group discussion was not feasible, although the approach may provide additional valuable information.
Conclusion
The self-management practice of hypertensive patients is sub-optimal. Patients have poor adherence to medications and lifestyle adjustments. The reasons for this are multifaceted. Although several individual patient issues relevant to the self-management of hypertension, including low awareness on the effectiveness of antihypertensive medicines, belief in traditional medicine, religious and social barriers were identified, facility-level problems were mainly responsible for poor self-management practice.
Generally, they could not get the required support from the health facility. It is hard for patients to get all the prescribed medicines in the hospital stock. They could not also receive appropriate education and counseling on the nature of the disease, medication adherence, and lifestyle modifications. Patients have fears about the caring, empathetic, and compassionate attitude of health care providers towards them. Even they have experienced disrespect, intimidation, and were insulted by health care workers.
The findings of the present study can help to plan effective interventions for the reduction of the identified barriers and to improve the self-management practice of patients with hypertension. The results suggest the need for a redesign of the education and counseling approaches for patients attending the chronic care clinic. The role of health care providers is essential in ensuring adequate adherence to physician recommendations.43In essence, it is important to set strategies like training of health care providers to enhance the patient-provider relationship and communication. Improving the availability of supplies of hypertensive medication in public facilities is also paramount for better medication adherence.
