Introduction
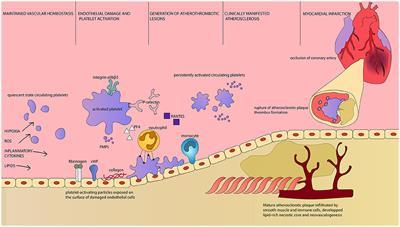
Obstructive sleep apnea (OSA) is a syndrome characterized by partial or complete obstruction of the upper airways, resulting in intermittent hypoxia, variably accompanied by sleep fragmentation and daytime sleepiness.1In male participants of the Swiss HypnoLaus cohort, the prevalence of moderate-to-severe OSA was 49.7%,2with 74.7% men aged 40 or over having OSA syndrome according to ICD-3 criteria.3However, OSA is often underdiagnosed and unrecognized in clinical settings.4OSA has been implicated in the development of cardiovascular conditions,5however OSA during rapid eye movement (REM) sleep and the resultant nocturnal hypoxemia are also longitudinally associated with cardiovascular disease6and associated risk factors such as hypertension,7insulin resistance,8metabolic syndrome,9and carotid atherosclerosis.10Animal models suggest that this increased cardiovascular risk is the result of intermittent hypoxemia11leading to activation of the sympathetic nervous system, increased oxidative stress12and systemic inflammation.13,14Furthermore, chronic intermittent hypoxia (CIH) reduced clearance of triglyceride-rich lipoproteins and inhibited adipose tissue lipoprotein lipase activity.15
Current studies investigating an association between OSA and dyslipidemia have shown inconsistent results.16–18This variation may be due to differences in study populations, the use of polygraphy rather than polysomnography, which may underestimate OSA, and studies largely conducted in the clinical setting which may not be generalizable to community-based, non-clinical samples. In a large clinical sample of adults being investigated for OSA, Trzepizur et al19showed a relationship between oxygen desaturation index (ODI) with higher triglycerides and lower HDL. In the European Sleep Apnea Database Cohort (ESADA), hyperlipidemia was independently associated with ODI20and a positive relationship between triglyceride concentration and both ODI and AHI were shown.21A recent study also showed an independent association between severe OSA (AHI ≥30/h) with dyslipidemia, total cholesterol and LDL cholesterol, with ODI shown to be an independent determinant of triglyceride levels.22In a general population sample, HypnoLaus Study investigators found that OSA was an independent risk factor for incident metabolic syndrome mediated through increased nocturnal hypoxemia, however no associations with incident metabolic syndrome components including high triglyceride or low HDL levels were seen.23
Given the paucity of community-based studies, we aimed to determine the association between polysomnography-measured OSA parameters and nocturnal hypoxemia with serum lipid concentrations in a community dwelling cohort (n=753) of adult males. Community-based studies are required which can identify atypical/asymptomatic OSA in individuals perceived to be at low risk of OSA and its associated cardiometabolic sequelae in those who are less likely to be referred for a sleep study. We hypothesize that given that central obesity is a strong risk factor for both OSA24and dyslipidemia, it may overwhelm any contribution of nocturnal hypoxemia to dyslipidemia. A few small clinical studies report lipid alterations in patients with OSA free of generalized obesity23or with both normal BMI and normal waist circumference levels.25,26Supporting this, a recent study using early morning 3-T-1H-magnetic resonance spectroscopy of the vastus lateralis muscle in men reported substantial and most likely transient increases of intramyocellular and extramyocellular lipids in non-obese men with OSA compared to participants without OSA.27Consequently, we conducted analyses stratified by waist circumference to observe an obesity-independent association between OSA metrics and dyslipidemia.
Materials and Methods
Participants were from the Men Androgens Inflammation Lifestyle Environment and Stress Study (MAILES study, n=2563 at baseline), a longitudinal study of community-dwelling men participating in the North West Adelaide Health Study (NWAHS) and Florey Adelaide Male Aging Study (FAMAS). Participants were aged at least 35 years at baseline (2002–2006) and are of predominantly European or Australian descent (96%) as previously described.28MAILES participants underwent a computer-assisted telephone health interview (CATI) in 2010 (n=1629), and men who did not report a previous diagnosis of OSA on a sleep study (n=1445) were invited to take part in a sub-study including polysomnography with 75.2% agreeing. In 2010–11, 837 men successfully completed eight-channel in-home unattended polysomnography (PSG, Embletta X100, Embla Systems, Broomfield, CO, USA) which measured EEG, EOG, EMG, nasal pressure, thoracic and abdominal effort, oximetry, and body position. Trained staff visited study participants in their homes to set up the PSG equipment. The Pittsburgh Sleep Quality Index29and the Epworth Sleepiness Scale30were administered, and all current medications were recorded. Sleep study participants showed minor healthy volunteer bias but did not differ in sleep symptoms compared to non-sleep study participants.28
Sleep studies were manually scored by a single, trained sleep technician according to American Academy of Sleep Medicine 2007 alternate criteria (hypopnea defined by a > 50% decrease in nasal pressure (or in both thoracic and abdominal excursions) with an associated 3% oxygen desaturation or an EEG arousal) and recommended for use in prospective epidemiological studies by the AASM and by an expert panel of the Australasian Sleep Association.31Independent variables included the apnea–hypopnea index (AHI), rapid eye movement sleep AHI (AHIREM, in participants recording at least 30 minutes of REM sleep),7AHIREMif AHINREM<10, and oxygen desaturation index (ODI, 3%). OSA was defined as AHI≥10/h of sleep, with further categorization into mild (AHI 10–19/h sleep), moderate (20–29/h sleep) or severe (≥30/h sleep) as defined by the alternate 2007 AASM definition.32The cut-offs for classification were chosen because Ruehland et al32have shown that an AHI of 5/h of sleep used to define sleep-disordered breathing scored by the 2007 recommended AASM criteria is equivalent to an AHI of 10/h of sleep using the alternate AASM definition, and 15/h using the older 1999 Chicago criteria. In order to maintain comparability with previous work a cut-off of 10/h was chosen.32
The study was conducted in accordance with the Declaration of Helsinki. Study approval was provided by the research ethics committees at the Royal Adelaide Hospital and North West Adelaide Health Service (approval numbers: 2010054, 02305H). Written, informed consent was obtained from all participants.
Lipid measurements were obtained at clinical assessments between 2007 and 2010 on a fasting blood sample taken between 8am and 11am after a 12 hour fast. Total cholesterol, triglycerides, HDL (high-density lipoprotein), LDL (low-density lipoprotein), glucose and HbA1c were quantified by an Olympus AU5400 automated chemistry analyzer28in two laboratories of the South Australian Department of Health pathology service.
Clinic assessment (as previously described)28included anthropometry and blood pressure. Body mass index (BMI, Kg/m2) was categorized by World Health Organization criteria of underweight/normal <24.9, overweight 25.0–29.9 and obese ≥30.0. Systolic and diastolic blood pressures were taken using a standard calibrated sphygmomanometer, with two measurements taken 5 to 10 minutes apart and the mean result calculated. A definition of systolic blood pressure >140 mmHg and diastolic blood pressure >90 mmHg or the use of anti-hypertensive medication was used to define hypertension. The presence of cardiovascular disease (including myocardial infarction, stroke, transient ischemic attack, angina) was identified via self-reported questionnaire. The presence of diabetes was defined by a doctor's diagnosis, HbA1c ≥6.5%, fasting glucose ≥7.0mmol/l or use of anti-diabetic medications.
Socioeconomic factors including age, gender, marital status, country of birth, highest education level and gross household income were obtained by CATI or self-completed questionnaire. Behavioral risk factors including smoking status and alcohol consumption were identified using a self-reported questionnaire and physical activity was assessed with the Active Australia questionnaire.33Current use of psychotropic agents (benzodiazepines, opiates, anti-psychotics, anti-depressants) and other sleep disrupting medications (nicotine replacement therapy) was identified on the night of the sleep study by staff.28Lipid lowering therapies were classified using the ATC classification system34C10A included plain lipid modifying agents (HMG-CoA reductase inhibitors, fibrates, bile acid sequestrants, nicotinic acid and derivatives, other lipid modifying agents) and C10B combinations of lipid modifying agents (HMG-CoA reductase inhibitors in combination with other lipid modifying agents). Depression was assessed using the 20-point Centre for Epidemiological Studies Depression Scale (CES-D) for NWAHS participants35and the Beck Depression Inventory (BDI-1A) for FAMAS participants.36
Principal component analysis was used to identify dietary patterns using data collected by a validated food frequency questionnaire. We identified two dietary patterns – western and prudent dietary patterns.37A prudent dietary pattern is based on high dietary intake of vegetables, fruit, fish, whole grains, legumes. A western dietary pattern is based on high intake of red meat, processed meat, refined grains.38We then used a single diet construct, derived by subtracting factor scores of prudent patterns from western pattern. A higher diet score represents higher adherence to a healthy diet.39
Statistical analysis was conducted using SPSS version 24 (IBM corporation, Armonk, NY USA). The analytical sample is described as mean ± SD or median and interquartile range (IQR) for continuous variables and n(%) for categorical variables and tests for differences across waist circumference categories included Student’s t-test, independent samples Kruskal–Wallis test and Pearson chi-square tests, respectively. Statistical significance was set at p<0.05. Those using psychotropic agents (benzodiazepines, opiates, anti-psychotics, anti-depressants) and other medications that disrupt sleep (nicotine replacement therapy) were excluded (n=84) from the analysis. The selection of the analytical sample (n=753) is shown in a CONSORT diagram (Figure 1).
Figure 1 Flow diagram of the MAILES study participants. *Sleep-disrupting medications include benzodiazepines, opiates, nicotine replacement therapy, anti-psychotics, anti-depressants. |
Linear regression analysis identified unadjusted, and covariate adjusted relationships between sleep parameters including AHI, AHIREM(in participants recording at least 30 minutes of REM sleep), AHIREMif AHINREM<10, ODI (3%) and lipid measures (Model 1). Separate models determined the association between sleep parameters and lipid measures, adjusted for age, waist circumference, smoking (non/former compared with current), alcohol (non-low risk compared with moderate-very high risk), total sleep time, diet, depressive symptoms (none compared with at least mild depression) and HbA1c (Model 2). We checked for collinearity and homoscedastic assumptions. Waist circumference was used rather than BMI due to evidence that it is a better predictor of cardiovascular risk compared to BMI.40
We further conducted a sensitivity analysis to exclude participants on lipid-lowering therapies. Given the effects of obesity on OSA and lipid levels, we further explored the relationship between triglycerides and AHI, AHIREM, AHIREMif AHINREM<10, and ODI (3%), stratified by waist circumference <95cm, 95–100cm and over 100 cm. Triglycerides were specifically analyzed due to a strong relationship between waist circumference and triglycerides, likely mediated through insulin resistance41and due to the minimal effects of lipid lowering therapies compared to other lipid measures. We further conducted binary logistic regression to determine associations between clinical categories of OSA [no OSA <10/hr, mild (10–19/hr), moderate (20–29/hr) and severe (≥30/hr) (27)] and the categorized dependent variable – triglyceride (≥ 1.7mmol/L). Covariates were the same as for the linear regression models.
Results
The sociodemographic and sleep characteristics of the analyzed sample overall and by OSA severity category are shown in Table 1. The mean (SD) age was 60.8 (10.9) years and waist circumference 99.3 (11.6) cm. The prevalence of diabetes was 17.1% and hypertension was 55.4%. Undiagnosed OSA (AHI≥ 10/hr) was determined in 52.6% of participants, with severe OSA (AHI ≥30/h) present in 12.4%. The characteristics of the sample in relation to waist circumference levels are shown inSupplementary Table 1.
Table 1 Demographic, Socioeconomic, Cardiometabolic Conditions, and Sleep Parameters of Study Sample |
Covariate unadjusted and adjusted analyses showed no significant associations of AHI, AHIREM, REM sleep predominant AHI (AHIREMif AHINREM<10), or ODI with lipid measures (Table 2).
Table 2 Multiple Linear Regression Analyses of the Association Between Measures of Nocturnal Hypoxemia and Lipid Profiles in Men (n=728§) |
In a sensitivity analysis (n=566), excluding participants using lipid lowering therapies (Table 3), there was no associations between ODI, AHI, AHIREM, or REM sleep predominant AHI (AHIREMif AHINREM<10) with lipid measures in co-variate unadjusted or adjusted analyses.
Table 3 Multiple Linear Regression Analyses of the Association Between Nocturnal Hypoxemia Measures and Lipid Profiles in Men without Use of Lipid Lowering Therapies or Sleep Disrupting Medications§(n=566) |
In analysis stratified by waist circumference to minimize the contribution of obesity to hypertriglyceridemia, triglyceride levels were positively associated with AHI, ODI and REM-AHI in participants with a waist circumference of <95cm (Figure 2) in co-variate adjusted analyses (p<0.05). Associations were not observed in participants with a waist circumference of 95–100cm or >100cm. When we considered AHIREMin participants with AHINREM<10, the association with triglyceride levels did not persist in men with waist circumference <95cm [unstandardized B (SE) =0.004 (0.008), p=0.60, n=147]. The results remained unchanged in men with waist circumference 95–100cm [−0.029 (0.016), p=0.076, n=47] and waist circumference >100cm [0.003 (0.009), p=0.75, n=118].
Figure 2 Forest plots for the association between triglycerides and AHI, REM-AHI and ODI in males separated into groups by waist circumference (<95cm, 95–100cm, >100cm). Coefficients are unstandardized with 95% confidence intervals. Model adjusted for age, smoking, depression, alcohol risk, total sleep time, HbA1c, diet quality. Sleep disrupting medications include benzodiazepines, opiates, nicotine replacement therapy, anti-psychotics, anti-depressants. |
In analyses based on clinical categories of OSA and triglycerides, in males with a waist circumference <95cm, severe OSA was significantly associated with an increased likelihood of triglyceride levels ≥1.7 mmol/L [OR=4.1 (95% CI: 1.1–15.5, p=0.039)]. For men with moderate OSA, there was an increased likelihood that did not reach statistical significance [OR=2.1 (95% CI: 0.7–5.9, p=0.17)]. Consistent with the findings of the linear regression analysis, there were no associations of severe OSA with triglyceride ≥1.7 mmol/L in men with waist circumference levels of 95–100cm [OR=0.9 (95% CI: 0.2–4.1, p=0.84)] and >100cm [OR=0.7 (95% CI: 0.4–1.5, p=0.40)].
Discussion
These data show that in a large, extensively characterized cohort of community dwelling men with a mean age of 61 years, after adjustment for covariates, there was no overall significant relationship between any measure of OSA metrics and serum lipid profiles. However, after stratification by waist circumference, AHI, ODI and AHIREMwere significantly and positively associated with serum triglyceride concentrations only in men without central adiposity.
OSA during REM sleep is characterized by longer obstructive events, with greater oxygen desaturations42and there is an increasing body of evidence43,44suggesting that compared to obstructive events during non-REM sleep, events during REM sleep may be more harmful. REM-predominant OSA has been associated with incident hypertension,7,45cardiovascular disease,46,47and glycemic control in type 2 diabetes.48In the current study, we were unable to demonstrate a separate contribution of AHIREMindependent of AHINREMto triglyceride levels. There may be a few reasons for this; REM sleep comprised only 15% of the sleep time in our study, there may be insufficient hypoxic burden present overall if significant OSA is not present in NREM sleep. Furthermore, to allow adequate observation of REM sleep, we excluded subjects with less than 30 min of REM sleep from AHIREManalyses. This may have excluded participants most at risk of chronic intermittent hypoxia-related lipid abnormalities given that severe OSA, or a high frequency of OSA arousals during the REM period will result in very short REM sleep.
Our findings regarding AHIREMare consistent with a recent clinical cohort study by Xu et al,49showing that associations of AHIREMwith increasing serum triglyceride concentration were not independent of AHINREM. A small study (15 participants) undertaken in Hungary showed that serum lipid profiles were not adversely affected by the presence of REM predominant OSA.50
Our findings also support other small clinic-based patient samples where OSA has been shown to be independently associated with serum triglyceride concentrations in individuals with BMI <30 Kg/m2,23and in patients with both normal BMI and normal waist circumference levels),25,26but not with obesity.51Of lean patients assessed as having OSA (AHI >5/hr and relevant symptoms), 39.6% had multiple metabolic abnormalities, including serum triglycerides ≥1.7 mmol/L.26In studies of lean participants25,52with varying severities of OSA ranging from mostly mild,44to mild to severe OSA,40compared to the control patients without OSA, those with OSA were significantly more likely to demonstrate impaired glucose metabolism and insulin resistance.
Animal studies provide evidence for a mechanism linking CIH and lipid abnormalities. In mice, CIH, as occurs in OSA, has been shown to have adverse effects on lipid metabolism including increasing hepatic triglyceride production, decreasing plasma triglyceride clearance by lipase activity inhibition and increased free fatty acid mobilization from adipose tissue.15,53Li et al found that lean, but not obese mice, with pre-existing abnormalities of lipid metabolism, exposed to intermittent hypoxia exhibited upregulation of key transcription factors involved in triglyceride biosynthesis (SREBP – sterol regulatory element-binding protein, SCD-1- SREBP-1 regulated enzyme for lipid biosynthesis).54Insulin inhibits hepatic triglyceride production and animal studies have also demonstrated a link between intermittent hypoxia and insulin resistance in lean mice.55,56In human studies, Koenig et al27recently reported large overnight CIH-related increases in plasma triglycerides that occurred in non-obese participants with OSA compared to participants with obesity and OSA (214.7 ±40.9 cf 95.6 ± 12.6 mg/100mL), and speculate that muscle or liver free fatty acid uptake capacity may be exceeded by overnight increases in circulating FFAs and may therefore be associated with re-esterification of FFAs. In a small clinical study of 15 “healthy” men with severe OSA (mean WC: 97cm, BMI: 28.4 kg/m2; free of significant comorbidities), Drager et al57reported disturbances in triglyceride-rich lipoprotein metabolism, with correction of delayed fractional clearance rates (FCR) of radiolabeled triglycerides and cholesteryl ester by 3 months of CPAP therapy supporting their earlier work.15That disrupted sleep that occurs in OSA is linked to dyslipidemia is further supported by a recent multi-ancestry genome-wide sleep-by-single nucleotide polymorphism (SNP) analyses on three lipid traits (HDL, LDL, and triglycerides) which identified gene-short sleep interactions that explained 4.25% of the variance in triglyceride levels.58
We therefore suggest based upon our data and the results of animal and mechanistic studies that intermittent hypoxia due to OSA may induce metabolic derangements associated with insulin resistance that cannot be separated from the predominant effect of visceral obesity and therefore results are observed in lean participants where obesity does not have a dominant effect. Supporting this, CPAP therapy has resulted in an improvement in insulin resistance in non-obese participants to a greater effect than in obese participants.59
The current study has several strengths. The participants were randomly recruited, community-dwelling men with extensive phenotypic, clinical, and biochemical assessments. They were broadly representative of the Australian male population aged 40 and over. The sleep subgroup was randomly selected from the whole study population, had similar socio-demographic and health-related characteristics to the full sample and gold standard polysomnography was performed in-home.28We adjusted for co-founders that were clinically relevant or showed strong significance in univariate analysis, and we performed sensitivity analysis excluding the use of lipid lowering agents. The cross-sectional nature of the study limits any inferences about causality, and the findings cannot be generalized to younger men or women. Sex-specific relationships between OSA and serum lipid profiles have previously been reported.60Furthermore, our findings from a cohort of community-dwelling men with many reporting few symptoms may not be generalizable to patients in the clinical setting. However, the advantage of population-based studies is the ability to identify healthy weight, asymptomatic individuals with OSA and cardiometabolic risk who would otherwise be unlikely to be referred for a sleep study.
Our findings have potential clinical implications. OSA has been shown to occur in approximately 5–14% of lean men61who may be perceived as being at low risk of OSA and its related cardiometabolic sequelae. The presence of obstructive sleep apnea should be considered in the workup for elevated serum triglycerides in lean men. A recent clinical study reported high prevalence rates of metabolic risk in lean patients with OSA (AHI >5/hr, BMI <25 kg/m2and waist <80cm in females; <90 cm in males), with dyslipidemia demonstrated in 61%, and two of three metabolic syndrome components in 64%.62Despite this high metabolic risk, treatment of hyperlipidemia in clinical populations with OSA is not high [eg 12% in the European Sleep Apnea Database Cohort (ESADA) cohort].20
OSA treatment with continuous positive airway pressure (CPAP) therapy, however, may not yield desired reductions in lipid levels and mainstay therapy with HMG-CoA reductase inhibitors and fibrates will be required. As reviewed recently,18,63observational studies and randomized controlled trials (often limited by small sample sizes and short follow-up times) have reported inconsistent effects of CPAP therapy on lipid parameters. In the ESADA Cohort, where higher ODI and AHI were associated with lipid parameters,20,21an observational study of at least 3 months of PAP therapy (n=1564) in the cohort yielded a mean decrease in total cholesterol of 4.9 mg/dl (0.13 mmol/L) after ≥3 months therapy, with no effect on triglyceride levels.64Compliance with CPAP therapy may have influenced the inconsistent benefits on lipid parameters reported in studies to date as CPAP use less than 4hrs per night is unlikely to treat REM sleep OSA demonstrated in our study and others to be relevant for lipid measures.49
In conclusion, we have shown that in a population of community-dwelling male adults, severe obstructive sleep apnea is a risk factor for raised serum triglyceride concentrations in those without central adiposity. This is likely the direct consequence of chronic intermittent hypoxia on triglyceride metabolism. Good CPAP compliance over the entire night including REM sleep may be beneficial. Further studies are required to evaluate the relationships between OSA and dyslipidemia in lean women and in younger men and to determine the effects of CPAP on triglycerides.
