The human gut is a robust ecosystem composed of a dynamic microbial community, collectively termed microbiota, which have important roles in the acquisition of energy from foods and the regulation of host physiology through immune modulation1,2. The finely tuned equilibrium between the host and microbiota may be disrupted when changes in the latter, described as “dysbiosis”, occur in the context of prevalent disorders such as obesity, diabetes and metabolic inflammation2,3.
Bacteria are the most abundant components of the human gut microbiome1,4,5. The composition of distal gut microbiota is known to be altered in obesity and obese individuals generally harbour a decreased ratio of Bacteroidetes to Firmicutes1,2,4. The relationship between gut microbiota and the emergence of obesity4,6,7might be causal, opening a myriad of possibilities for novel treatment approaches.
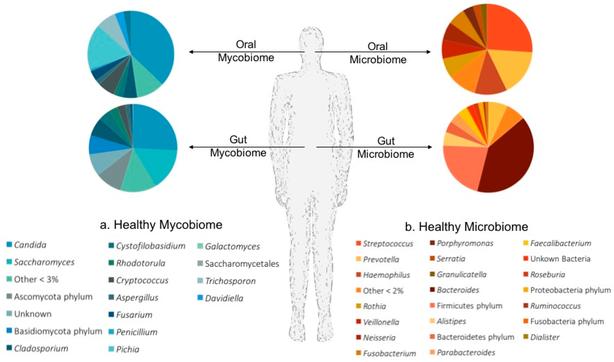
The mycobiome, referring principally to the fungal component of microbiota, comprises approximately 0.03–2% of total gut microorganisms and is an integral part of the gastrointestinal tract8,9,10,11. The diversity of fungi inhabiting the human gut remains poorly explored9,12,13,14. A fungal cell is >100-fold larger than a bacterial cell and thus fungi represent substantially greater biomass than is suggested by the number of available genomes3.
Next generation sequencing has been valuable for characterizing the human gut mycobiome3,12,15,16. Studies have shown that the human gut is home to more than 66 genera and 184 species of fungi, with Candida, Saccharomyces and Cladosporium being particularly common3,9,11,12,15,17,18. In mice, the majority of gut fungi are indigenous to the intestine since only a few of the most common gut fungi were found in mouse food16.
Mycobiome dysbiosis is relevant in inflammatory diseases such Crohn’s disease or ulcerative colitis16,17,18. As yet, no studies have addressed the role of gut fungal microflora in obesity and related diseases.
Here, we used Multitag Pyrosequencing (MTPS) to evaluate fungal diversity in faecal samples from obese and non-obese patients using internal transcribed spacer (ITS) primers, which have broad fungal specificity. We found that the faecal mycobiome is disturbed in obese patients in comparison with non-obese subjects, in parallel with alterations in glucose and lipid metabolism. We observed an optimal grouping of individuals according to genus abundance, that clustered together with metabolic phenotypes. Additionally, we found a dynamic relationship between adiposity and the gut mycobiome after weight loss, indicating that manipulation of gut mycobime communities could be a novel approach in the treatment of obesity.
